Written by Kirsten Steinman
Edited by Nicki Steinberger, Ph.D.
EDITOR’S SUMMARY: Reproductive health is shaped long before a positive test. Nutrient intake, hormonal balance, and daily habits all influence the quality of eggs and sperm. From folate, omega-3s, and vitamin D to sleep, movement, and limiting alcohol and caffeine, these core factors can tip the scale toward stronger fertility and a healthier pregnancy.
Let’s say you’ve spent years growing your career, investing in relationships, and creating a life you love. Now, you finally feel ready to take that next big step—starting a family. But suddenly, the conversations change. Friends are undergoing in vitro fertilization (IVF), spending thousands on fertility treatments, or quietly struggling for years to conceive. Naturally, you start to wonder: Will it be that hard for me too? Tracking ovulation apps, counting fertile days, and peeing on sticks can start to feel like a full-time job. Each passing month without a positive pregnancy test can make optimism harder to hold onto. You’re not alone. Today, at least one in six women and one in seven couples face infertility. According to Pew Research, a full one-third of Americans either know someone—or are themselves—seeking help to get pregnant.
But what if your fertility story doesn’t have to start in a clinic—and the most important steps toward conception begin before you ever track a cycle? Mainstream medical sources cite several contributing factors to rising infertility rates, including delayed parenthood, increasing rates of sexually transmitted infections, and reduced frequency of gynecologic care. Roughly 20% of women wait to have their first child after age 35—a time when egg quality begins to decline, increasing the risk of genetic abnormalities and reducing the likelihood of carrying a pregnancy to term. Why does female fertility decline at all? Much of the answer comes down to hormone balance. A fertile woman produces optimal levels of estrogen and progesterone throughout her menstrual cycle, triggering ovulation and preparing the uterus for implantation. Women with imbalances in luteinizing hormone and follicle-stimulating hormone—both produced by the pituitary gland—may not ovulate consistently, or at all.
Yes, infertility is on the rise, but not always for the reasons you might expect. Many people conceive naturally for the first time in their late 30s and 40s without difficulty. And it may not be luck or genetics—research shows these women often share certain patterns: optimal vitamin D levels, good overall health, anti-inflammatory eating habits, absence of chronic medical conditions, regular outdoor exposure, consistent physical activity, and stable, supportive relationships. In truth, fertility is shaped by something far more empowering than luck. It’s deeply connected to lifestyle—what you put into your body, how you move, your sleep quality, and yes, even the products you use every day.

Food Quality, Packaging, and Fertility Risks
What you eat—and how it’s packaged—can directly influence your ability to conceive
The road to conception isn’t paved with convenience foods and sugary indulgences. To support hormone production and reproductive function, your body thrives on whole foods, steady energy, and essential nutrients. Processed foods, on the other hand, contribute to inflammation, strain the adrenal glands, disrupt blood sugar, and elevate cortisol—all of which can lead to insulin resistance and excess estrogen, delaying ovulation and throwing your cycle out of sync. That doesn’t mean everything has to be made from scratch—minimally processed options such as frozen fruits and vegetables, plain whole yogurt, nuts and seeds, and BPA-free canned staples like beans, tomatoes, or salmon can still be part of a healthy diet. Stick to whole foods that are essentially one ingredient, and when it comes to packaged items, look for short, recognizable ingredient lists. Be mindful of added sugars, limit iodized (table) salt, and season freely with high-quality sea salt.
Even with a diet rich in whole, nutrient-dense foods, less obvious factors can interfere with fertility. Gluten is one such example. Integrative physician and midwife Dr. Aviva Romm warns that gluten sensitivity—whether from celiac disease or non-celiac gluten intolerance—can be a hidden factor in fertility challenges:
“Celiac disease and possibly even non-celiac gluten intolerance, can affect fertility, increase miscarriage risk, and is associated with additional pregnancy complications; it also plays a role in endometriosis, leaky gut, and Hashimoto’s, all of which can impact fertility and pregnancy. So go gluten free – not only until you conceive – but at least until you’re a year postpartum, because gluten can also affect your thyroid postpartum, and this can contribute to challenges with milk production and also contribute to postpartum anxiety or depression.”
Beyond individual food triggers, the way food is stored and packaged also plays a role in fertility health. Ultra-processed foods (UPFs) are often wrapped in plastics containing chemicals such as phthalates and bisphenols—known endocrine disruptors. These compounds can interfere with sex hormones and have been linked to reproductive issues in both children and adults—especially when exposure occurs during early development. One study, “Ultra-processed foods intake and sex hormone levels among children and adolescents aged 6–19 years: a cross-sectional study,” found clear associations between UPF consumption and altered hormone levels:
“Additionally, during the production and packaging of UPFs, there may be increased exposure to various chemicals, including phthalates, bisphenols, per- and polyfluoroalkyl substances (PFASs), organophosphate, acrylamide, and micro(nano) plastics. Phthalates, bisphenols, PFAS, organophosphates, and micro(nano) plastics are recognized as endocrine disrupting chemicals, which may affect sex hormone levels. Acrylamide has been classified as a probable human carcinogen and has also been found to disrupt sex hormone homeostasis among preschool-aged children and youths aged 6–19 years.”
Phthalates are widespread—not just in food packaging, but in personal care products, cosmetics, and even cleaning supplies. These endocrine disruptors bind to estrogen receptors, mimicking or blocking the hormone’s effects and disrupting hormonal balance. Research has linked phthalates to endometriosis, a painful condition in which tissue similar to the lining of the uterus grows outside the uterus. These chemicals may also interfere with follicle development and impair the ovaries’ ability to produce essential hormones. To reduce exposure, choose products labeled “BPA-free” and “phthalate-free,” limit processed foods, and opt for unscented or naturally scented (essential oils only) personal care and cleaning products.
Men aren’t immune to fertility challenges—in fact, male factors contribute to nearly half of all infertility cases, with diet playing a central role. High consumption of cured meats (containing added nitrates/nitrites and/or antibiotics), sugary drinks, and refined grains has been linked to lower sperm quality and reduced fertilization rates. Conversely, a nutrient-rich diet—abundant in antioxidants (from fruits and vegetables), whole grains, wild seafood, 100% grass-fed meat and dairy, omega-3 fatty acids, and folate (found in dark leafy greens and liver)—can help improve sperm concentration, motility (ability to swim), membrane fluidity, and even reduce DNA damage. Keep in mind, sperm take about 72 days to fully mature, so dietary changes may take a few months to show results.
Mercury-containing fish are another fertility disruptor for both women and men. Mercury can accumulate in the testes and ovaries, suppressing enzymes essential for sperm production and causing breaks or abnormal numbers in chromosomes. These effects can lead not only to infertility, but also to birth defects and pregnancy loss. Swordfish, king mackerel, and tuna are especially high in heavy metals, which can deplete zinc and disrupt testosterone and progesterone levels. Instead, choose smaller fish that are lower on the food chain and typically have less mercury, such as sardines, anchovies, wild salmon, herring, or trout.
Microplastic contamination is an increasing concern in seafood, especially as these particles accumulate up the food chain. One study found that 75% of commercial species contain microplastics as a result of industrial and consumer waste dumping. An estimated 50 trillion to 75 trillion pieces of plastic now pollute the world’s oceans, making up nearly 80% of all marine pollution. These tiny plastic particles, small enough to contaminate plankton and fish larvae, can reduce sperm count, impair DNA integrity, and disrupt the blood-testis barrier—a structure in the testes that separates developed germ cells from the bloodstream. They may also interfere with ovarian function, embryo development, and hormonal balance. You can reduce your overall exposure by avoiding canned foods that aren’t labeled BPA-free, using glass or stainless steel containers, not heating food in plastic, and filtering tap water. Other hidden sources include synthetic clothing such as polyester and nylon, chewing gum, and household dust.
To reduce heavy metals and harmful substances that have accumulated in your body, support detox pathways by eating foods that help neutralize free radicals—unstable molecules produced during the body’s detoxification process. Antioxidants, found abundantly in plants and also in some meats, poultry, and fish, can help prevent the damage caused by these unstable chemicals. Some of the most antioxidant-rich choices include berries, dark leafy greens, beets, artichokes, pecans, walnuts, dark chocolate (80% cacao or higher), and herbs such as oregano, thyme, and turmeric. Certain animal foods also provide antioxidants, including wild salmon, pasture-raised poultry, grass-fed beef, and organ meats like liver.
Also include cruciferous vegetables such as cauliflower and broccoli; sulfur-rich foods like onions and garlic; and high-fiber options like chia seeds and flaxseeds. Chlorella, cilantro, and healthy fats from avocado, grass-fed butter, tallow, ghee, and extra virgin olive oil can also support toxin removal. Hydration is essential—mercury is excreted in urine—and sweating through exercise or saunas can help as well. Probiotics support the gut microbiome, helping rid the body of unhealthy substances while limiting mercury absorption.
Protein is vital, but more isn’t always better—especially when it comes to fertility. High intake has been linked to hormone imbalance, ovulatory infertility, inflammation, imbalances in gut bacteria, estrogen dominance, insulin resistance, and irregular periods. According to the U.S. Department of Agriculture, women should aim for 46 grams of protein per day, or roughly 10% to 35% of daily calories. To put that in perspective, 7 grams of protein are found in just 1 ounce of lean meat, 2 ounces of cooked beans or tofu, 1 tablespoon of nut butter, or a single egg. It’s also worth noting when tracking daily intake that protein isn’t exclusive to animal products—most whole foods contain at least a small amount.
On the other hand, some nutrition experts consider the USDA’s minimum recommendation extremely low—especially for active individuals or those focused on building or maintaining muscle mass, which is not only key for blood sugar regulation but also tied to long-term vitality and physical resilience. Preserving lean muscle supports insulin sensitivity, joint stability, and overall hormone balance—factors that influence both your general health and your ability to conceive.
The American College of Sports Medicine, as cited by Mass General Brigham, recommends 1.2 to 1.7 grams of protein per kilogram of body weight per day for active people—about 0.5 to 0.8 grams per pound. For example, if your ideal body weight is 130 pounds, you might aim for 65 to 104 grams of protein per day. This higher range can help stabilize blood sugar, preserve lean muscle, and promote satiety. Signs you may be consuming too much protein include bad breath, frequent urination, dehydration (as the kidneys work harder to process excess nutrients), digestive issues, and even weight gain—all of which can affect hormone balance and, over time, fertility. To keep intake balanced, focus on healthy fats, fresh fruit, thoughtfully sourced meats, and reasonable portions.
When it comes to fertility nutrition, dairy can be a double-edged sword. While it provides protein and calcium, research shows that for some women—particularly those who are lactose intolerant or have sensitivities—regular consumption may have pro-inflammatory effects. Dairy products contain insulin-like growth factor and female sex hormones, which can stimulate testosterone production and worsen hormonal imbalances. Some studies have also linked dairy intake—especially low-fat varieties—to a higher risk of polycystic ovary syndrome (PCOS), a condition that disrupts normal ovulation (often due to hormonal imbalances and the development of ovarian cysts).
If you experience bloating, cramping, or other digestive discomfort after consuming dairy, consider eliminating it for a few weeks and observing how you feel. Is your skin clearer? Do you feel less moody? When you decide to reintroduce dairy, start with full-fat and fermented products such as yogurt and kefir. These are often better tolerated and may be more supportive of fertility due to their higher fat content and gentler impact on blood sugar regulation. Choose organic, grass-fed, and preferably pasture-raised dairy to minimize exposure to added hormones, antibiotics, and pesticide residues, while supporting better nutrient content and animal welfare. Raw dairy, when available from a trusted source, may also be less inflammatory and easier to digest for some people, thanks to its natural enzymes and unaltered fat structure. Ultimately, if you find that dairy isn’t a good fit for your body, there are plenty of calcium-rich alternatives to support reproductive health. Tahini, chia seeds, dark leafy greens, and organic non-GMO tofu are all nourishing choices.
Whole foods are generally a better choice than supplements for meeting nutrient needs. While supplements can help fill gaps, they often contain isolated nutrients in synthetic forms that your body can’t metabolize efficiently. In some cases—particularly with excessive use—supplementation may increase the risk of kidney stones, liver disease, and even certain cancers. Meanwhile, fruits and vegetables deliver a rich array of phytochemicals and other plant-based compounds that can’t be replicated in a pill. Animal proteins like meat and fish provide highly bioavailable nutrients that are readily absorbed and utilized by the body.
A well-rounded, varied diet is the best way to meet your needs—if your plate is full of color, you’re on the right path. This is especially important for fertility, as whole foods provide the complex synergy of vitamins, minerals, and antioxidants needed to support hormone production, egg and sperm quality, and a healthy reproductive system. When thoughtfully chosen, high-quality supplements may be added later to correct deficiencies and support proactive, preventive care.

Nutrients That Make a Difference
Some building blocks quietly shape hormone balance, egg quality, and sperm health long before conception
One of the most important nutrients for fertility is folate (vitamin B9), found in leafy green vegetables, citrus fruits, legumes, egg yolks, beef liver, and certain types of seafood, including clams, oysters, and wild-caught salmon. A study of women trying to conceive in the United Kingdom, New Zealand, and Singapore, “Maternal B-vitamin and vitamin D status before, during, and after pregnancy and the influence of supplementation preconception and during pregnancy: Prespecified secondary analysis of the NiPPeR double-blind randomized controlled trial,” found that 90% had marginal or low levels of this vitamin. Folate supports cell growth, helps protect against early pregnancy loss, and reduces the risk of neural tube defects such as spina bifida and anencephaly when taken around the time of conception. In men, it is essential for sperm DNA synthesis and methylation.
Unfortunately, many prenatal vitamins contain folic acid—a synthetic version of folate that must be converted by the liver and other tissues into a usable form. Because this conversion process isn’t always efficient, folic acid may build up in the bloodstream, which has been linked to several potential issues: masked vitamin B12 deficiencies, impaired fetal growth, and gestational diabetes. Naturally occurring folate, on the other hand, is readily metabolized and used by the body and poses no risk of overdose. To avoid synthetic forms, be mindful of processed foods such as cereals, tortillas, and breads that are fortified with folic acid. If you do need a supplement, look for methylated folate (often listed as L-methylfolate or 5-MTHF, short for 5-methyltetrahydrofolate) for better absorption and bioavailability.
Omega-3 fatty acids, particularly docosahexaenoic acid (DHA), help regulate hormones, improve sperm and egg quality, boost blood flow to reproductive organs, reduce inflammation, and support embryo implantation. In men, DHA is essential for maintaining sperm membrane fluidity as well as the function and development of the acrosome, the cap-like structure that enables sperm to penetrate the egg. Cod liver oil—a traditional, food-based source of omega-3s that also provides fat-soluble vitamins A and D—can be a potent addition to a fertility-focused routine. A high-quality algae-based supplement can also help bridge the gap—many fertility specialists recommend more than 2,000 mg of DHA per day for optimal support. Most people fall short on omega-3s from diet alone, but there are plenty of nutrient-rich sources to choose from. These include sardines, wild-caught salmon, chia seeds, flaxseeds (freshly ground is best), hemp seeds, grass-fed meats and dairy, and pasture-raised eggs.
While many nutrients support fertility across the board, certain micronutrients play a particularly important role in male reproductive health. Zinc supports testosterone production and sperm formation and is found in oysters, beef, pumpkin seeds, and cashews. CoQ10 fuels mitochondrial energy in sperm cells and is especially abundant in organ meats like heart and liver, as well as in sardines and spinach. Selenium acts as a powerful antioxidant, protecting against oxidative stress and DNA damage, and is found in high amounts in Brazil nuts and eggs. While tuna also contains selenium, it’s best to limit intake or choose lower-mercury options such as skipjack or pole-caught varieties. Including these nutrients in your diet—or supplementing when needed—can significantly improve sperm quality and overall fertility outcomes.
Another key player is choline, a nutrient essential for fertility and early development. This often-overlooked compound supports healthy egg and sperm membranes, influences methylation (a process that helps regulate gene expression), and plays a major role in early brain and neural tube development. Eggs are one of the richest natural sources of choline, along with liver, wild salmon, and cruciferous vegetables. Adequate intake before and during pregnancy is critical, since demand increases significantly and deficiencies are common. As noted in “The Optimal Fertility Diet,” Dr. Aviva Romm emphasizes:
“It’s no wonder eggs are a symbol of fertility. Eggs provide choline, essential for baby’s brain development, and eggs are an especially rich source. They’re also an excellent source of blood-sugar balancing protein and energy. Is eating two eggs daily too much? Absolutely not – there’s ZERO connection between eggs and heart disease.”
Vitamin D is another non-negotiable. It regulates progesterone and estrogen in women, supports menstrual regularity, and influences testosterone and sperm levels in men. Sunlight is the best source—aim for about 20 minutes a day on each side of the body, exposing as much skin as possible—but food sources such as egg yolks and UV-exposed mushrooms can also help. Because melanin reduces vitamin D synthesis, you may need more sun exposure if you have darker skin or live at a higher latitude. Functional medicine practitioners often recommend maintaining a vitamin D blood level between 50 and 80 ng/mL. If you’re not within this range through sun exposure and diet alone, consider supplementing with food-based vitamin D3 combined with K2 for better absorption and calcium balance.
If sunscreen is part of your sunlight routine, it’s worth looking more closely at what’s in the bottle. Ingredients like oxybenzone, homosalate, octocrylene, and octinoxate can act as hormone disruptors, creating imbalances in estrogen and progesterone that may affect ovulation, menstrual regularity, and sperm quality. Protect your endocrine system by covering up with clothing and wearing a hat instead. You may also consider skipping sunglasses at times, as they block UV rays needed for vitamin D production and can interfere with hormones that regulate sleep and metabolism. To boost melanin production and build a “solar callus,” try spending time outside before 10 a.m.
Vitamin C may not be the first nutrient that comes to mind for fertility, but its role is both vital and far-reaching. Research shows the ovaries have an increased demand for and uptake of vitamin C, which supports optimal ovulation and healthy uterine function. One of its most important roles is stimulating the production of luteal hormones, particularly progesterone, which helps prepare the endometrial lining for implantation. Vitamin C is equally important for male fertility—inadequate levels can compromise sperm function and lead to significant sperm loss.
To naturally boost your intake, prioritize organic, seasonal fruits and vegetables, which offer the highest levels of this nutrient. Excellent sources include cherries, guavas, plums, and red, green, and yellow peppers. Keep in mind that vitamin C is heat sensitive, so some potency can be lost through cooking or steaming. An added benefit: vitamin C enhances the absorption of non-heme iron from plant foods, which supports oxygen delivery to reproductive tissues and helps prevent anemia during pregnancy.
Lifestyle Factors That Influence Fertility
Your daily habits—from medications to sleep patterns—can work for or against your reproductive health
While nutrients play a powerful role in supporting fertility, it’s equally important to consider what might be creating barriers. Many common medications—including NSAIDs, steroids, antibiotics, and some antidepressants—can interfere with reproductive hormones by altering hormone production, disrupting ovulation, or affecting the menstrual cycle. Contraceptives, in particular, can have lingering effects. About 65% of women ages 18 to 49 use some form of birth control, and while oral contraceptives leave the system relatively quickly, long-acting methods such as injectable contraceptives—like Depo-Provera—may delay a return to fertility for a year or longer. If you’re planning to conceive, discuss potential timelines for fertility return with your doctor before starting or stopping any contraceptive method. It’s also important to consider how other aspects of health—especially mental health—can play a role in reproductive outcomes.
Mental health is often an overlooked piece of the fertility puzzle. Conditions like anxiety and depression can influence hormonal balance, and in some cases, certain drugs—such as selective serotonin reuptake inhibitors and tricyclic antidepressants—may have an impact on ovulation or sperm quality. Around one in ten women trying to conceive are currently taking these pharmaceuticals. While medication can be an important part of managing mental health, it’s worth recognizing the role lifestyle plays. Simple, supportive practices such as spending time outdoors, engaging in regular movement, eating nourishing foods, and maintaining strong social connections can positively influence mood and overall endocrine function—and may even enhance the effectiveness of other treatments. These habits can also create a healthier internal environment for conception and pregnancy.
Caffeine is a hot topic. The American College of Obstetricians and Gynecologists considers up to 200 milligrams per day to be safe—that’s about one 12-ounce cup of brewed coffee. However, some fertility experts recommend avoiding it entirely. High caffeine intake can alter estrogen levels, potentially leading to irregular menstrual cycles and inconsistent ovulation. This can make it harder to predict your fertile window and may lower your chances of conception. Caffeine can also harm egg health, interfere with implantation, and may increase the risk of early pregnancy loss or affect fetal development in the early stages. Men may want to skip that second cup as well, since caffeine can influence testosterone and sperm production.
To naturally reduce reliance on caffeine, it can help to explore underlying factors like poor sleep, stress, or overexposure to artificial light. These often drive the need for an energy boost in the first place. It’s also worth noting that ground coffee can harbor mold species such as Penicillium and Aspergillus, which may pose additional health concerns. If you do choose to drink coffee, opt for organic beans, and when selecting decaf, look for options processed with the Swiss Water method, which avoids chemical solvents
Alcohol can be particularly disruptive. It promotes infertility by altering the balance of hormones that regulate menstruation and ovulation, sometimes preventing ovulation from occurring at all. Even occasional drinking can interfere with hormone balance, which means moderation alone may not be protective when you’re actively trying to conceive. High consumption—eight or more drinks per week for women and 15 or more for men—and frequent binge drinking are especially damaging, linked to gonadal atrophy in men (testicular shrinkage), reduced sperm count, and poor sperm motility. In women, alcohol can impair egg quality and, during pregnancy, is associated with an increased risk of heart defects in developing babies. Experts generally recommend that anyone trying to conceive avoid alcohol, whether doing so with a partner or using a donor. The good news: fertility often begins to improve within a few months of stopping alcohol use, especially when paired with a nutrient-rich diet and healthy lifestyle habits.
While reducing harmful exposures is key, so is nurturing the body through positive practices. Regular movement can lower stress, improve hormone regulation, enhance insulin sensitivity (critical for those with PCOS), and boost circulation to reproductive organs. Moderate exercise also helps regulate menstrual cycles and makes it easier to track ovulation. If you’re not sure where to start, walking is powerful medicine—low impact, joint-friendly, beneficial for immune function and heart health, and nearly impossible to overdo.
Working toward a daily target of 7,000 steps—about 3 to 3.5 miles—is ideal for supporting hormonal balance. Begin by tracking your current daily steps, then aim to add 1,000 to 2,000 steps—this could be a short 15-minute walk or taking the stairs more often. After a few weeks, add another 1,000 to 2,000 steps, perhaps by incorporating a morning or evening walk, strolling during phone calls, or taking a lap around the block after meals. Make your walks more enjoyable by going with a friend or listening to a podcast. A step tracker can help keep you motivated.
Squats throughout the day can help regulate blood sugar, as the glutes and quads play a key role in glucose uptake. They also strengthen the pelvic floor and core muscles, which are essential for supporting a growing uterus. Squats further boost blood flow to the reproductive organs, supporting overall fertility. Starting a daily workout routine can feel challenging—especially if your hormones are out of balance, even in ways you might not realize. Conditions that disrupt hormone levels are often linked to inflammation, which can sap your energy and make movement feel harder than it should. That’s why finding simple, accessible ways to stay active throughout the day can help set you up for long-term success. Try doing a set of squats while waiting for your tea to steep, during TV commercial breaks, or before sitting back down at your desk—small bursts really do add up.
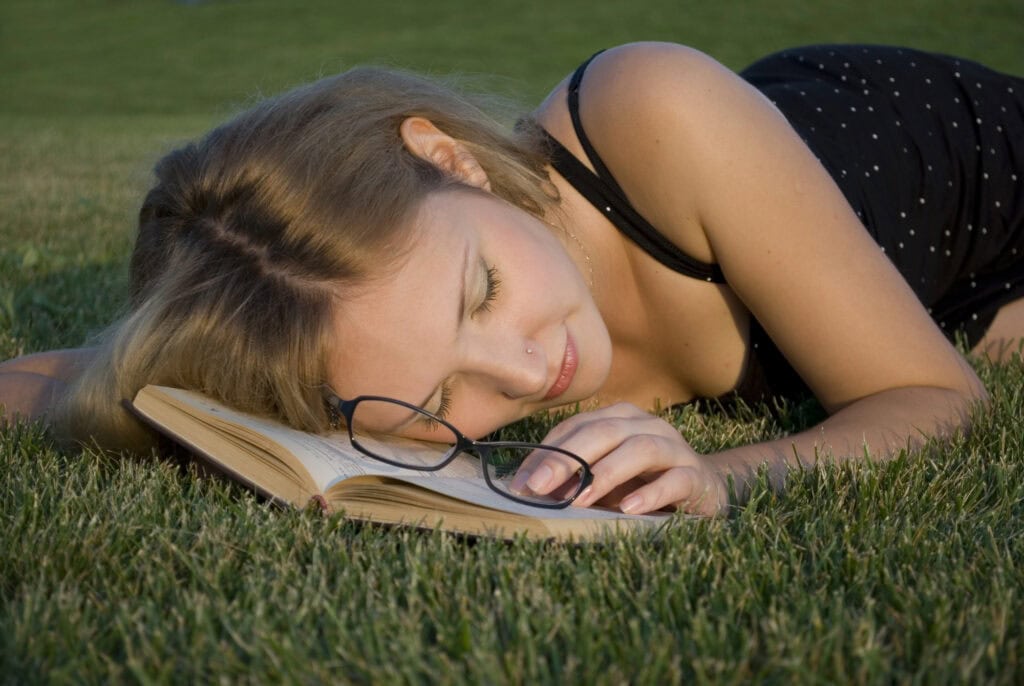
Sleep is a fertility superpower—and skipping it can cost you. Too little rest disrupts melatonin (the sleep hormone), cortisol (the stress hormone), growth hormone, and progesterone. It also interferes with the production of gonadotropin-releasing hormone, which controls luteinizing hormone and follicle-stimulating hormone—two key players in ovulation and sperm production. Women who get fewer than seven to nine hours may face irregular cycles, weight gain, mood swings, low libido, and greater risks of fertility or pregnancy complications. In men, poor sleep can lower testosterone and reduce sperm quality. Sleep isn’t a luxury—it’s a biological necessity. Support better rest by avoiding late meals (finish eating two to three hours before bed), limiting alcohol and caffeine in the evening, cutting screen time at least two hours before bed, wearing blue-light blocking glasses once the sun goes down, keeping your room dark, quiet, and cool, and staying active during the day.
Supporting fertility isn’t just about getting pregnant—it’s about building the healthiest foundation possible. With IVF costs reaching $20,000 per cycle—not to mention the emotional rollercoaster of hormone shots, daily ultrasounds, and an uncertain outcome—it makes sense to support your body before turning to medical intervention. Fertility reflects your body’s overall balance, resilience, and vitality. And while not every infertility journey can be resolved through lifestyle changes, many can. With the right foundation, your body can work at its best. So take the walk. Get the sun. Cook the meal. Clear the toxins. Ditch the perfume. Nourish your hormones and your mind. Because when you align with what your body truly needs, you’re not only increasing your chances of conception—you’re setting the stage for a thriving, joyful transition into parenthood.
~
Published on August 21, 2025.
If you’ve found value in this article, please share it!
To support the research and health education of AVFC editorial, please consider making a donation today. Thank you.