EDITOR’S SUMMARY: In Western mainstream medicine, osteoporosis, a disease resulting in weak and brittle bones, is typically treated with chemical pharmaceuticals. With an eye on symptom-reduction in an attempt to prevent bone fractures and falls, via drugs, little attention is given to the root cause, and even less toward a holistic approach to reversal. As with all medications, mild to severe “side effects” are a consideration. Accordingly, as with all health conditions, including this associated decrease in bone mineral density, how you live your life, i.e., the choices you make day-to-day play a major role.
By Verity Bell
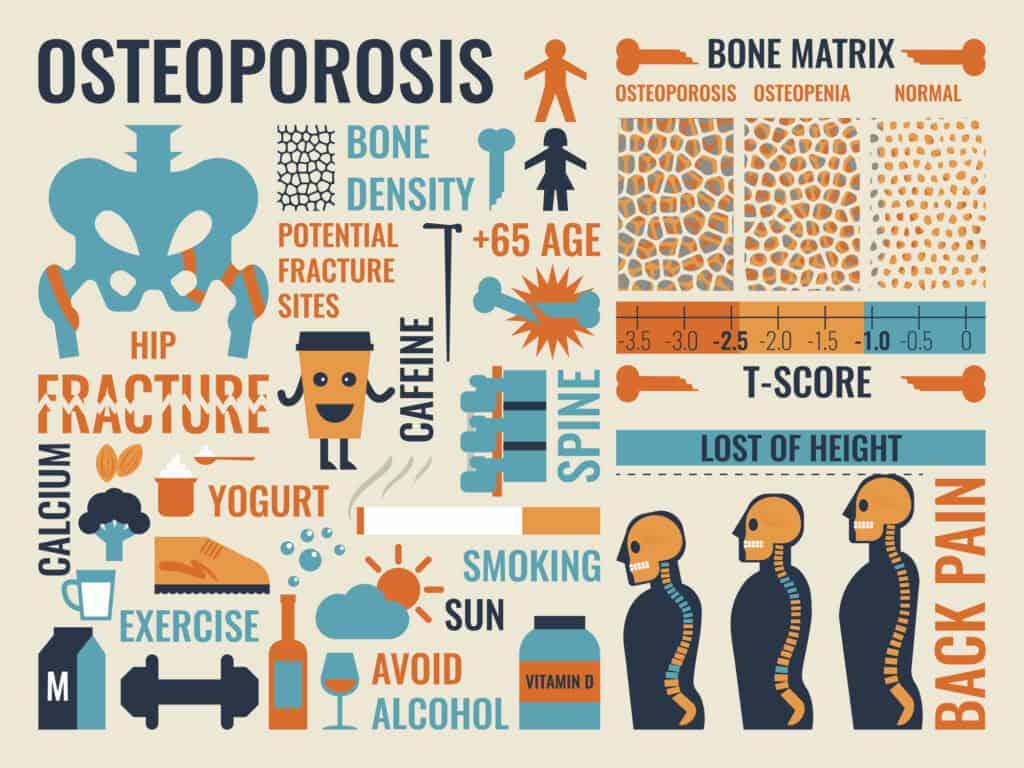
If you’re a woman over 50 years old, chances are you will be encouraged by your doctor in good faith to get a bone density screening for osteoporosis. After all, should you fracture a hip (the worst case scenario), you could develop blood clots from prolonged immobility, and possibly not recover your ability to walk. The one year mortality rate, in fact, for hip fractures is estimated to be over 20%. At the same time, modern medicine and the interests of the pharmaceutical industry have become so intertwined in recent years, that there are certain things you might benefit from being aware of before deciding how to approach this. As its name suggests (“osteo” referring to bone, and “por” to pore), osteoporosis is characterized by bones that have become porous enough to fracture in response to very little stress. Some deterioration in bone quality occurs naturally with age, but the diagnosis of osteoporosis is given when that deterioration happens faster than normal. At its most advanced stage, it results in fractures, and may involve loss of height, or a stoop if it affects the spine.
Various contributing factors have been identified as causes of osteoporosis, including lack of weight bearing exercise, low vitamin D, hormone level depletion, chronic inflammation, mineral deficiency, stomach acid deficiency, pharmaceuticals, and toxins. Among the pharmaceutical culprits are steroids, opioids, thiazolidinediones (for diabetes), SSRI antidepressants, anticonvulsants, and proton pump inhibitors. Ironically, proton pump inhibitors are prescribed to treat acid reflux, which is a side effect of the bisphosphonate medications commonly used to treat osteoporosis. The National Institute on Aging estimates “… about one in five women over 50” are diagnosed with osteoporosis, along with “… one in 20 men.” As A Midwestern Doctor pointed out in the article, “The Great Osteoporosis Scam,” for drug-makers, such a market represents a business opportunity not to be passed up. The article illustrated how the industry generates “sales funnels” by exploiting patients’ needs and fears, then steers you toward false solutions that invariably do more harm than good. The funnels begin with screening measures based on misleading diagnostic criteria that induce you to take medications, which often have questionable efficacy, as well as adverse effects.
Diagnostics and Allopathic Medications
The trouble with the scans: In the case of osteoporosis, the screening measures are called dual x-ray absorptiometry, or DXA scans. Their purpose is to measure bone mineral density (BMD), and they do this in terms of standard deviations from that of a healthy young adult, as expressed by “T-scores.” A T-score below -2.5 is enough to qualify for a diagnosis of osteoporosis, while the runner-up prize (for those between -1 and -2.5) is osteopenia (the risk of developing osteoporosis). One of the issues that have been identified with this technology is a propensity for error. For example, there are variations in results between machines, procedures, and even bones measured. But the overwhelming problem with its use is that focusing on bone mineral density to the exclusion of other factors is misleading. From Empower: Total Health, Robyn Chuter explained:
“Many low-impact fractures occur in people with normal or high BMD, while many people with low BMD will never suffer a fracture,” because “Reduced bone mineral density is just one risk factor for low-trauma bone fracture.”
Osteoporosis, Chuter explains, used to be “defined as an enlargement of the spaces of bone (Haversian canals) whereby a porous appearance is produced” but the widespread adoption of this technology, which does not detect such spaces, has “changed the definition.”
The extent to which the focus on bone mineral density distorts the prognostic picture is underscored by the following excerpt from The British Columbia Office of Health Technology Assessment report:
“BMD measurements are poor predictors of whether individual women will suffer future fractures. In fact, most women will be misclassified if they are sorted according to BMD scores. In fact, most women who will suffer a hip fracture (the most consequential fracture) will be classified as normal when compared with the mean (average) BMD of women the same age. If women more than one standard deviation (SD) below the mean are classified as being at increased risk for fractures, then 70% of the women who will eventually suffer fractures will not come from the group identified as being at risk. At the same time, only half of the 30% of women labeled as being at increased risk will have a fracture. The other half will receive unnecessary treatment.”
Sales funnels: This non-essential treatment, or from industry’s perspective, an expanded market, is of course the purpose for which a sales funnel exists. So who created this, and how did they go about it? National Public Radio (NPR) journalist, Alix Spiegel investigated this question. From “How A Bone Disease Grew To Fit The Prescription”: “It’s the story of how the definition of what constitutes a disease evolves, and the role that drug companies can play in that evolution.” It is a story that begins with Kate Benghauser, a former marathon runner with bone density “just a hair away from that of the average healthy 30-year old” who was prescribed medication for osteopenia (alongside 3 out of 4 of her co-workers over 50). Despite being “extremely health conscious,” Spiegel remarks, Benghauser had never heard of osteopenia. This is hardly surprising because prior to 1992 when the category was created during a World Health Organization (WHO) conference, neither had anyone else.
Cited in the article was a professor of medicine who attended the conference. She admitted that the parameters for osteopenia were decided on in a somewhat arbitrary fashion. She then goes on to add that there was no intention for it to be regarded as a condition to be treated. And this may be true of certain participants, but whether it was true of all involved is open to debate. Here are two pieces of circumstantial evidence to consider: As Susan Kellerher of the Seattle Times observed, the conference was “sponsored by two large drug companies and a drug-company foundation,” and the parameters established are broad enough to “include more than half of all women over 50.” You can decide if these two factors are causally or coincidentally connected.
But the sales funnel story related in Spiegel’s article does not end there. By 1995, Merck had launched its osteoporosis drug, Fosamax, which it was struggling to sell due to lack of widespread, affordable access to scans. So they hired consultant Jeremy Allen to solve the problem. Allen established a subsidiary called the Bone Measurement Institute (of which he happened to be the sole employee). He then pressured existing companies to shift from larger, more expensive machines that measured the spine and hips to smaller “peripheral” ones that only measured wrists, arms, heels, and fingers. Manufacturer Richard Mazess of Lunar Corp., a highly successful company, claimed he was threatened with reprisals when he objected, on the basis that peripheral scans would be a poor predictor of more serious fractures. Merck’s next move was to buy out another company in order to demonstrate the new business model. It subsequently funded trials for peripheral machines, launched a massive marketing campaign, and ultimately secured the passage of the 1997 Bone Mass Measurement Act (BMMA). This was the clincher because it led to insurance companies reimbursing patients for scans, and doctors for machines, turning the whole thing into a profitable venture. All in all, in the words of the authors of “Selling sickness: the pharmaceutical industry and disease mongering”:
“… the medicalisation of reduced bone mass—which occurs as people age—is an example of a risk factor being conceptualized as a disease.”
“Drug companies have sponsored meetings where the disease was being defined, funded studies of therapies, and developed extensive financial ties with leading researchers. They have funded patient groups, disease foundations, and advertising campaigns (on both drugs and disease) targeted at doctors and have sponsored osteoporosis media awards offering lucrative prizes to journalists.”
Bisphosphonates: If the treatment Merck was trying to sell was innocuous, and the loss no more than financial, the sales funnel might not be so alarming, but sadly, this was not the case. Bisphosphonates, the main class of osteoporosis medications (of which Fosamax is one) have an impressive array of side effects. The list includes: gastrointestinal irritation, esophageal ulceration, esophageal cancer, eye inflammation, debilitating musculoskeletal pain, kidney deterioration, osteonecrosis of the jaw, and spontaneous fractures of the femur (thigh bone). You heard that right … spontaneous fractures. This might leave you scratching your head, but when you understand the mechanism of action it begins to make more sense. Bisphosphonates increase bone density by suppressing the cells that break bone down. But in so doing, they also suppress turnover (or renewal). Since breakdown is a prerequisite for renewal, when old bone cannot be broken down and replaced, it becomes brittle. In short, equating density with resilience and health, seems to some extent to be a misconception. These drugs, although administered for three to five years, can remain in your system for ten or more after cessation, which means that side effects (including pain) can take a long time to subside. And to compound the issue, your doctor may not even recognize the pain as an effect of the medication, attributing it instead to the condition.
Many sources, even those who caution against the use of bisphosphonates for osteopenia, will still champion or defend it for osteoporosis based on purported efficacy. However, on closer inspection, the greatest efficacy demonstrated was in the prevention of subclinical vertebral fractures (“subclinical” meaning that the fracture was discovered on an x-ray, rather than as a result of the patient experiencing pain). In the case of hip fractures, on the other hand, it prevented no more than one in a hundred. This was noted by David Newman, M.D., in his summary and review of the scientific literature. He then astutely called attention to the industry sponsorship of the studies, citing:
“A long history of selective outcome reporting, selective publication, occasionally fraudulent reporting and dubious methodological choices” as reasons to “scrutinize and doubt” their “optimistic claims.”

Managing (and Preventing) Osteoporosis With Lifestyle
Fortunately, there is some good news: Many of the factors that contribute to the condition can be remediated through lifestyle change in conjunction with an integrative practitioner. You can learn how to minimize toxins in your diet, personal care products, and immediate environment, start a resistance exercise program, and address deficiencies (including hormonal ones) with whole foods and supplementation. While taking estrogen may be avoided due to its associations with cancer, progesterone, which appears to be non-carcinogenic, has been found to be protective. One way to supplement minerals is by adding fulvic/humic acid to your water. Vitamin D deficiency is correctable as well, either through increased sun exposure (preferably) and/or supplementation, and low stomach acid may potentially be ameliorated via judicious use of a supplement called Betaine HCL.
Surprisingly, however (and contrary to the overwhelmingly ubiquitous general recommendation), caution may be advised when it comes to calcium supplementation. A Swedish study that followed 61,433 women for 19 years found that the group with the highest calcium levels (in the region of 1,591 mg) showed a 19% increased rate of hip fractures. The authors speculated this could be due to the reduction of bone turnover, as in the case of bisphosphonates. An editorial review of the literature, moreover, found that only two studies suggested a reduction in overall fractures from calcium supplementation by 10%. Conversely, there is evidence for a host of adverse effects including renal calculi (kidney stones), acute gastrointestinal issues and calcified arteries. One randomized control study referenced in the review found that as little as 600 mg of supplemental calcium increased all cause mortality in its elderly subjects by 47%, and cardiovascular mortality by 76%. In “Calcium supplements: bad for the heart?”the author of the editorial concluded:
“Thus, the consistent evidence is that calcium supplements do more harm than good and that other interventions are preferable for reducing the risk of osteoporotic fractures.”
The above review did not, on the other hand, find adverse effects with dietary calcium, and speculated that it could be beneficial. Since it is absorbed more slowly and in smaller quantities over time, it doesn’t circulate at high levels in the blood. Another thing worth knowing is that calcium can be obtained not only from dairy products, but also from dark, leafy vegetables (preferably raw or steamed) and canned fish (like sardines). If you are unable to get it from your diet, and feel that supplementation is your only option, combining it with Vitamins D3 and K2 may help mitigate the harms by helping to transport it where it needs to go.
Most sources will tell you that osteoporosis cannot be well-managed or reversed without potentially invasive treatments, including chemical medications and hormone therapy. Yet, anecdotal evidence seems to suggest that more may be achievable through natural means post-diagnosis than is commonly supposed. This was the experience of nutritional therapist, Phoebe Liebling, and functional medicine doctor, Lauryn Lax. Diagnosed with osteoporosis at 25, due to hormonal issues arising from her use of oral contraceptives, Liebling declined the conventional recommendations in favor of a holistic solution. Eight years later, when it was expected that her condition would have progressed, she no longer met the diagnostic criteria. Lax, likewise, was diagnosed at 23 after suffering from malnutrition due to anorexia, and navigated her way out of the osteoporotic density range within one year.
Liebling describes her protocol in terms of balancing the rate of bone renewal with bone breakdown by increasing the rate of renewal. Contrast this with the conventional approach, which she says, “freezes us in time” by arresting renewal in order to preserve mass. This renewal process is driven by weight-bearing exercise (to be prioritized over cardio, which can inhibit bone growth by triggering the stress hormone, cortisol). Equally important is the food you eat. To be specific, an anti-inflammatory diet rich in nutrients, minerals, and protein can provide the raw materials needed for bone creation. This refers to unprocessed, organic foods, containing a high ratio of omega-3 fatty acids (found in fatty fish and seaweed) relative to the omega-6 fats (found in “foods” such as grains, nuts and seed oils). Liebling recognized this approach required discipline and commitment proportional to the disadvantages you are facing (such as age, reduced hormone levels, and degree of bone degradation), but claimed it is effective to the extent it is embraced. Lax’s recommendations were similar, although she emphasized the importance of gut health for nutrient absorption, and included the following caveat with regard to exercise:
“ANY form of exercise done in excess (and/or without proper recovery) strips our bodies of nutrients and inhibits the optimal “repair” process of both muscle and bone tissue. Additionally, overtraining both elevates cortisol (our stress hormone), decreases estrogen production and suppresses stomach acid (essential for absorbing our nutrients from food), setting the stage for weakened bone health.”
The extent to which the results achieved by these women might be applicable across age ranges and demographics would be difficult to establish, as little science has been done to help determine it. However, two comparable cases are shared by physical therapist, Margaret Martin; one of which involves a woman of 70 years old. Martin also cites a study in which subjects in their 60s increased their bone mass by 2% following an exercise program, while that of the control group (no exercise program) decreased by 4%. Findings from the study, “Prescribing Physical Activity for the Prevention and Treatment of Osteoporosis in Older Adults,” based on the same age group were encouraging as well, as discussed in the following excerpt:
“An important goal for exercise trials is to assess efficacy in populations most at risk of fracture, yet limited studies have focused on older adults with, or at risk of developing, osteoporosis, with many excluding such individuals due to perceived safety concerns. However, an ongoing Australian study focused on post-menopausal women with low BMD (lumbar spine T-score < −1.0) has shown significant improvement in femoral neck (+2.8%) and lumbar spine BMD (+3.3%) during an eight-month supervised PRT [physical resistance training] intervention compared to an unsupervised home-based intervention [29]. These preliminary results highlight the effectiveness of PRT in older adults with poor bone health.”
The review’s authors stipulated that while the improvements noted may seem modest, bone mass density is only one of the risk factors for fracture, and that a 1–3% density increase may be as much as is needed to protect against it. They further pointed out that even beyond its contribution to bone density or health, the improvements to muscle strength and balance that exercise confers can reduce the risk of fractures by preventing falls. One final perspective that may be important to include is that of clinical nutritionist, Susan E Brown who advocates consuming an alkaline-promoting diet for osteoporosis prevention and treatment, stating:
“Unfortunately, we’ve strayed from the acid-alkaline balanced diet that our ancestors achieved. We favor meat, sugars, grains, low-mineral processed foods and other acid-forming foods, while consuming far too few alkaline-forming vegetables, fruits, nuts, seeds and other foods beneficial for bone. The net result is that our eating patterns create a condition known as “chronic low-grade metabolic acidosis.”
The hypothesis is that the body compensates for metabolic acidosis by pulling alkalizing minerals out of the bones in order to stabilize blood pH. It is one that mainstream science has tended to dismiss due to the fact that measurable changes in blood pH are not detectable in response to diet. As Joseph Pizzorno remarked in his article, “Acidosis: An Old Idea Validated by New Research”:
“Up until about 10 years ago, no research existed to counter this skepticism. However, since then, a growing body of research has documented not only that “acidosis” is a real phenomenon, but that it is now known to contribute to a wide range of diseases, such as metabolic syndrome, cancer, osteoporosis, kidney stones, and increased susceptibility to environmental toxins—and new research is adding to the list.”
Acidosis, Pizzorno explained, will only produce changes in blood pH when compensatory mechanisms have been exhausted, which “typically only happens in advanced disease like kidney and lung failure” but that “the pH in the cells and intracellular space becomes more acidic,” nonetheless. Excitingly, he goes on to say, not only is an alkalizing diet “consistently associated with greater bone density, but alkalinization through supplementation with potassium and magnesium citrates decreases urinary excretion of calcium, increases bone density, and decreases fracture.” In light of this information, it is interesting to note that a new osteoporosis drug candidate has a nanocarrier that uses bone pH as a trigger for the drug’s release. As researcher, Shyni Varghese put it, “Whenever you have a lot of bone degeneration, the pH is very low. The bone tissue is more acidic.”
The moral of the story is this: It’s never too late or too early to take your health (and healthcare) into your own hands. You must be your very best advocate, by saying “yes” or “no” strongly when making medical decisions. It is imperative you do your research to be fully informed of options and outcomes. It can also be extremely effective to have a friend or family member advocate for you/with you, as two voices may be stronger than one in a doctor’s office. A lifestyle approach to preventing and reversing disease, whether implemented on its own or integrated with Western medicine, starts with mindset. Once you feel confident about your direction, you’ll be far less likely to be swept along the conveyor belt of corporate captured consensus. If you choose to empower yourself by looking outside the box, you may be pleasantly surprised by what you learn. Paying attention to the food you eat, how you move your body, the thoughts you think, and the ways you can reduce stress will never steer you wrong.
~
Published on September 26, 2024.
If you’ve found value in this article, please share it!
To support the research and health education of AVFC editorial, please consider making a donation today. Thank you.

