EDITOR’S SUMMARY: In “Eye Health Part One: The Nutrition You Need to Protect and Restore Your Vision,” dietary nutrients, including antioxidants and omega-3 fatty acids were deemed necessary to improve vision and sustain optimal ocular health. Self-care goes a long way, and what you do at home matters. That said, it’s also important to be informed about eye doctors’ roles (and perspectives) in your healthcare, typical exam procedures, and choices you may need to make in your practitioner’s office.
Written by Carter Trent
Edited by Nicki Steinberger, Ph.D.
Whether you wear glasses or not, at some point in your life, you may have ventured into an eye clinic or medical center to get an eye exam. In fact, the American Optometric Association (AOA) recommends regular eye exams to be sure your eyes are healthy, and to catch signs of disease as early as possible. The AOA suggests adults over 19 years of age get tested at least once every two years by an optometrist or ophthalmologist, and annually if you’re over 65 years old.
Both of these vision specialists are qualified to perform exams and diagnose eye health, but possess different levels of training and expertise. Ophthalmologists are medical doctors who specialize in the eyes. Optometrists don’t attend medical school, and instead, earn a doctor of optometry (OD) degree from optometry school. An optometrist serves a similar role to your primary care doctor, as the one to go to for routine vision check ups. They perform tests to check your eye health, and determine a prescription for glasses if you need it. An ophthalmologist focuses on medical situations related to your eyes, including treating disease and performing surgeries, for example, to correct cataracts.
In the U.S., however, a shortage of both practitioners can make scheduling difficult, with long waits between initial and follow-up appointments. And while it might be said that a visit to the eye doctor is less daunting than a trip to the dentist, the thought of having your eyes dilated with stinging eye drops may bring about just a bit of anxiety. But what if you didn’t need a doctor after all? What if a machine could do the job more quickly with absolutely no pharmaceutical eye drops needed?
No-brainer? Perhaps … maybe not. Enter an artificial intelligence (AI) algorithm that’s ready for you at the eye clinic. One stop shop; no follow-up necessary for diagnosis, and you’ll receive a “yay or nay” for “diabetic retinopathy” immediately, from a retinol camera. This AI-based system has been approved by the FDA, and is growing in availability in medical centers across the nation. On the other hand, if you feel more comfortable being assessed by a human who is experienced in this area, that is certainly understandable.
A couple known drawbacks in choosing the AI-route for this diagnostic are as follows: 1. The algorithm specifically looks for and detects diabetic retinopathy only, therefore, other diseases may be missed. 2. The system is set up to err on the side of caution, so positive diagnoses may be handed out more generously than accurately.
From KFF Health News, “As AI Eye Exams Prove Their Worth, Lessons for Future Tech Emerge”:
“Digital Diagnostics, formerly Idx, received FDA approval for its system in 2018, following decades of research and a clinical trial involving 900 patients diagnosed with diabetes. It was the first fully autonomous AI system in any field of medicine, making its approval “a landmark moment in medical history,” said Aaron Lee, a retina specialist and an associate professor at the University of Washington.”
Now back to tradition … Your care provider will typically run you through a series of tests to evaluate your overall eye health, and to assess your visual acuity—the ability to clearly make out objects you’re looking at. In a routine exam, to evaluate functionality and the health of your eyes, the clinician will generally check your eye movement, peripheral vision, front and back areas of your eyes, color blindness, and eye pressure. Problems they look for include glaucoma—a disease damaging the optic nerve, and leading to vision loss—a torn retina, and hypertensive retinopathy—blood vessels in your eyes that are abnormal due to high blood pressure.
Conventional Eye Exam Tests Explained
To assess visual acuity (sharpness of vision), your clinician uses an eye chart. This is where you identify a series of letters or text that progressively get smaller as you read down the chart. Your provider measures your visual acuity based on how far down the chart you can read the characters accurately. Your visual acuity is measured as a fraction with 20/20 representing normal vision. If your vision is less than 20/20, you may need glasses to correct your sight. If that is the case, a retinoscopy test will be given to determine the prescription for your glasses. The retinoscopy exam involves a phoropter machine. This device allows your clinician to put different lenses in front of your eyes to measure the degree of refraction, which is how much power the lenses in your glasses should have to correct your vision.
In addition to visual acuity, your doctor will check your pupils, the black dots in the center of your eyeballs. Looking for normal functionality, a light will be shined in each eye to observe your pupils’ reactions. This area of your eyes naturally adjusts in size based on lighting conditions. The iris, which is the larger circle around your pupil that gives your eyes their color, uses tiny muscles to change the pupil’s size. In bright light, these muscles constrict to shrink the pupils, reducing the amount of light entering your eye. In the dark, your pupils dilate, or get bigger, to let in more light, allowing you to see more clearly.
Your optometrist or ophthalmologist will also examine the structure of your eyeballs, including eyelids, cornea, iris, and lens. This is done using a slit lamp, a magnifying mechanism showing an enlarged view of your eyes. As you place your face on a chin rest in front of the device to hold your head still, the clinician shines a slit-like beam of light at your eyes, looking for signs of damage or disease. You’ll also receive an ocular motility test to evaluate whether your eyes can follow a moving object normally. Ocular motility requires both eyes to move and work together to focus. You’ll be asked to track an item as it’s moved in front of you, such as the examiner’s finger. A visual field test is performed to check your peripheral vision since it’s possible to lose your side vision without noticing, which may be an early sign of glaucoma.
Different ways to execute this exam exist, such as the standard automated static perimetry test (SAP), and the kinetic visual field test. Both use a machine, called a perimeter. You’ll be asked to look at a computer screen showing you an object, such as a ball of light, that appears and disappears throughout different parts of the screen. As you click a button when you perceive the object, the perimeter tracks which objects you didn’t see. This allows your doctor to determine if there’s loss in your peripheral vision.
An eye pressure test, called tonometry, measures the fluid pressure in your eyes. Checking eye pressure is important because if it’s elevated, it can damage your cornea, the clear, outermost layer of your eye. Your cornea protects your eye from elements such as debris and germs. Elevated pressure could also be a sign of glaucoma. A common approach to tonometry is to blow a puff of air into each eyeball using a device called a tonometer. Your eye pressure is measured based on the time it takes for the air to bounce back to the tonometer.
An additional technique to test eye pressure is called applanation tonometry. This involves the clinician putting anesthesia drops in your eyes to numb them, and then touches them with a tiny probe, which measures the amount of resistance to pressure. An alternative method is rebound tonometry, where the tonometer uses a tiny plastic ball that bounces off your eye so quickly, you can’t feel it. Because it happens so fast, you don’t need anesthesia drops.
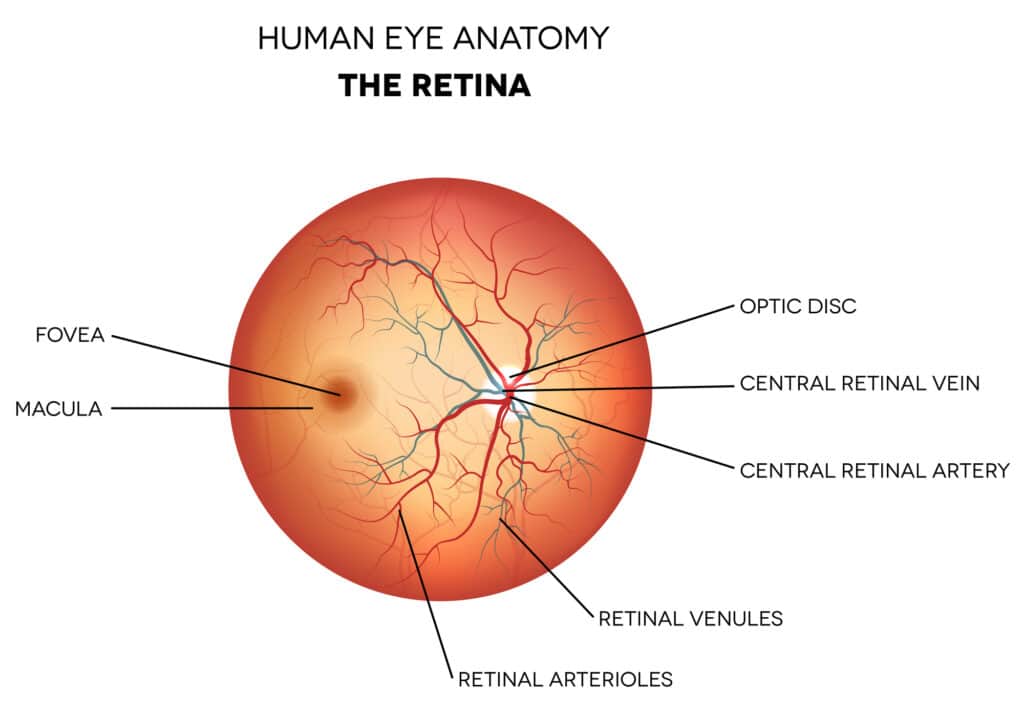
Your eye exam will include ophthalmoscopy, also known as fundoscopy. This checks the fundus, which is the back part of your eyeball. The fundus encompasses the retina, optic disc, blood vessels, and choroid. The choroid, which delivers nutrients to your inner eye, is the connective tissue and blood vessels between the retina at the back of your eye, and the white part around your iris. Ophthalmoscopy involves shining a light at each eye from a tool called an ophthalmoscope. This device uses tiny magnifying lenses to allow the examiner a good look inside your eye.

Because the ophthalmoscope’s light causes your pupils to contract, limiting what can be seen in the fundus, the practitioner will administer chemical drops into your eyes to cause mydriasis. This is when the pupils become fixed in a dilated position. By inducing mydriasis, your pupils remain as large as possible to give the care provider a wider line of sight into the back of your eyes. Once the dilating drops, called mydriatics, are inserted, it takes about 20 to 30 minutes for your pupils to fully dilate. Various drugs are available to induce mydriasis, such as cyclopentolate and tropicamide, and each works in a different way. Some eye drops cause mydriasis by paralyzing the sphincter muscle around your pupils to prevent them from contracting. At the same time, the drops activate contraction of the dilator muscle of your iris, which causes your pupils to dilate.
Other mydriatics, such as tropicamide, are anticholinergic, which means they block the activity of a neurotransmitter in your body that activates the muscles used to contract your pupil, causing paralysis in these muscles. The effects of mydriatics can last for some time, slowly subsiding in four to six hours. Because the drugs cause mydriasis, common side effects include sensitivity to light and blurred vision. One step you can take to minimize these adverse reactions is to ask for a lower dose of eye drops. Research reveals a lower dose is just as effective at producing mydriasis while reducing side effects.
If having mydriatics inserted into your eyes doesn’t sound appealing, technology offers an alternative called retinal imaging. This is where a machine scans your eyes and takes photos of them. However, not all providers or locations offer this, and you will typically have to ask and advocate for this option. Advancements in retinal imaging have occurred over the past 20 years, and today’s digital photos use what’s called ultra-wide field imaging (UWFI). UWFI is the most comprehensive imaging technology available, which enables the examiner to view up to 82% of your eyes, while traditional pupil dilation allows only 15%.
UWFI can complement or replace traditional pupil dilation, but one drawback is that it takes two-dimensional images. This is not ideal because your eyes are three-dimensional. That’s where another technology comes in, called optical coherence tomography (OCT). This technique takes cross-sectional images of the retina using light waves. When combined with UWFI, the two technologies provide a comprehensive, detailed view of your eyes. An additional technology is corneal topography. This is a test that produces maps of your cornea. Corneal topography involves resting your face against a bowl-shaped machine where you’re asked to watch digital images on a computer screen while the device takes three-dimensional pictures of your cornea. This machine can be used to ensure contact lenses fit the shape of your eyes.
An ophthalmologist can also use corneal topography to prepare for eye surgeries, such as LASIK vision correction and cataracts surgery. In addition, corneal topography can identify other issues, including changes in the shape of your cornea, to catch conditions such as keratoconus, where the cornea bulges out, causing blurred vision. While digital imaging offers benefits over pupil dilation, your insurance may not cover the cost. Be sure to check on this ahead of time so you don’t get a surprise medical bill in the mail. One final routine test involves checking for color blindness. This can be performed using the color plate test. Looking at a circle made up of different colored dots, each has a unique shape inside. The shapes you cannot see will identify your color vision deficiency.
An Eye Toward Holistic Ocular Diagnostics and Treatment
The source of the famous saying about your eyes being the windows to your soul is up for debate. But given the large degree your eyes reveal about your overall well-being, you could say they are the windows to your health. There are optometrists and ophthalmologists who practice holistic (whole person; not isolated, individual parts), functional (root cause of dysfunction/imbalance; not symptom-suppression), and integrative (natural medicine combined with allopathic) methods of vision care. This means they consider a multitude of factors affecting your eye health, including mental wellness, the food you eat, levels and types of physical activity, stress management, sleep patterns, and social relationships.
Here’s how integrative optometrist, Neda Gioia described the holistic approach to vision care.
“By recognizing the body as a complex system of interconnected parts, integrative medicine emphasizes the importance of identifying and addressing the root causes of health issues, rather than just treating their symptoms.”
She further elaborated by saying:
“I now recognize that many eye-related problems, such as age-related macular degeneration, cataracts, and glaucoma, have been linked to poor nutrition. By providing my patients with guidance on healthy eating habits and supplement options, I can help address the underlying causes of these conditions. I’ve also started to focus on stress management as a way to improve my patients’ eye health. Stress has been linked to a variety of health problems, including eye strain, dry eyes, and even vision loss. By providing my patients with relaxation techniques, such as meditation or deep breathing exercises, I can help manage their stress and improve their overall eye health.”
Because holistic practitioners understand your body is a unified system, they recognize your eyes can signal health issues that don’t just affect your vision or ocular health alone. These conditions may include high blood pressure, risk of stroke, arthritis, and signs of cancer. Optometrist William White described an example of this, stating, “People can feel absolutely fine, but high blood pressure has a cumulative effect.” He explained:
“We can see changes due to vascular conditions caused by diabetes or hypertension. The blood vessels in the retina can become a little more stiff and hardened. They’ll push on each other and cross, like two hoses in a confined space. When it gets really bad, we’ll see some of the blood vessels start to leak, we’ll see some hemorrhaging.”
Not only do integrative practitioners consider your overall health as part of vision care, they differ from traditional optometrists or ophthalmologists by way of their use of natural treatments, rather than relying solely on pharmaceuticals or invasive surgeries. For example, the tears from your eyes keep them moist and clean. If your body produces less of this fluid, you may experience discomfort known as dry eyes.A functional medicine clinician will address the root cause of your dry eyes, rather than treating the symptom alone. This might include recommending acupuncture to increase blood flow, and produce an anti-inflammatory response, or a heated eye massage to unclog tear ducts.
Integrative ophthalmologists and optometrists may also assess and treat your conditions by way of homeopathy. These practitioners have found value in using this modality for a variety of reasons:
- Healing their own imbalances through holistic practices
- Realizing drugs alone don’t get to the root of a health problem
- Learning that chronic conditions need the support of nutrition, physical activity, and sound sleep
- Understanding that decreasing daily toxics is critical to prevent as well as turn around disease
- Hearing patients’ desires to collaborate in their healthcare
- Knowing that chronic stress responses must be managed, and stress-reduction practices implemented
From ModernOptometry, “Introduction to Holistic Optometry,” the following doctors shared their insights. Regarding long-term medications, Eric J. Conley, OD, MJ, FAAO, said:
“I think the main concern that drives my interest is that many ocular health issues are chronic, especially those related to dry eye, and one solution, of course, is to keep people on medications, often for life, once they develop symptoms. But if you can find a way to avoid the need for long-term medication use, or at least minimize it, that’s a desirable outcome for many patients.”
Dr. Herring believes in offering her patients treatment options, and targeting root causes of illness:
“I like to give my patients options by offering alternative therapies, such as homeopathics and herbals, either alone or as adjunct therapy. I recommend clean products, meaning little-to no-toxins, wherever possible, and support therapies that target root causes. Simply addressing lifestyle factors and nutrition has also been at the core of my eye care, as these things have direct effects on our eyes. I am also planning to start offering virtual holistic eye care consults in the coming year.”
In speaking about the future of integrative optometry, Dr. Gurvich stated:
“Gut health, I would say, is the biggest one. The role our microbiome plays in our overall health is not a new concept, but there are more and more gut-x associations emerging lately. We know there is a gut-eye axis, but elucidating this further will bring light to a lot of ocular and systemic conditions.”
Final words from Dr. Conley regarding holistic optometry:
“I think a major take home is that we need to find an avenue to be able to get funding for non-medication products to really get buy-in from the health care community, because every doctor takes their oath seriously. Standard medicine in the United States is generally reactive, but we can adopt a mindset that is more proactive.”
As you can see, holistic, integrative, and functional approaches in the field of ocular health are expanding into the likes of many clinical practices. If these methods appeal to you, even as adjunct therapies, search out a practitioner who has incorporated natural medicine into their doctor-patient philosophy and protocols. To be well-informed, consider learning more about natural eye health on your own. This will also lend to a richer conversation with your eye doctor.
And regarding the use of AI diagnostics, realize that as a patient and consumer, you do have a choice. There is a tendency to believe you need to accept the tests and treatments your doctor (or medical scheduler) offers you. Understanding that you are a co-participant in your healthcare is important, and advocating for yourself (or another) is often necessary where traditional medical power hierarchy exists. If you feel unclear about how to move forward with a health decision, it could be worth getting a second opinion, or trying out a new practitioner or clinic. Above all else, allow your intuition to weigh in on giving you direction and guidance.
~
Published on June 13, 2024.
If you’ve found value in this article, please share it!
To support the research and health education of AVFC editorial, please consider making a donation today. Thank you.